Welcome to the Witherspoon Institute
Critical analysis of classic mistakes in medicine
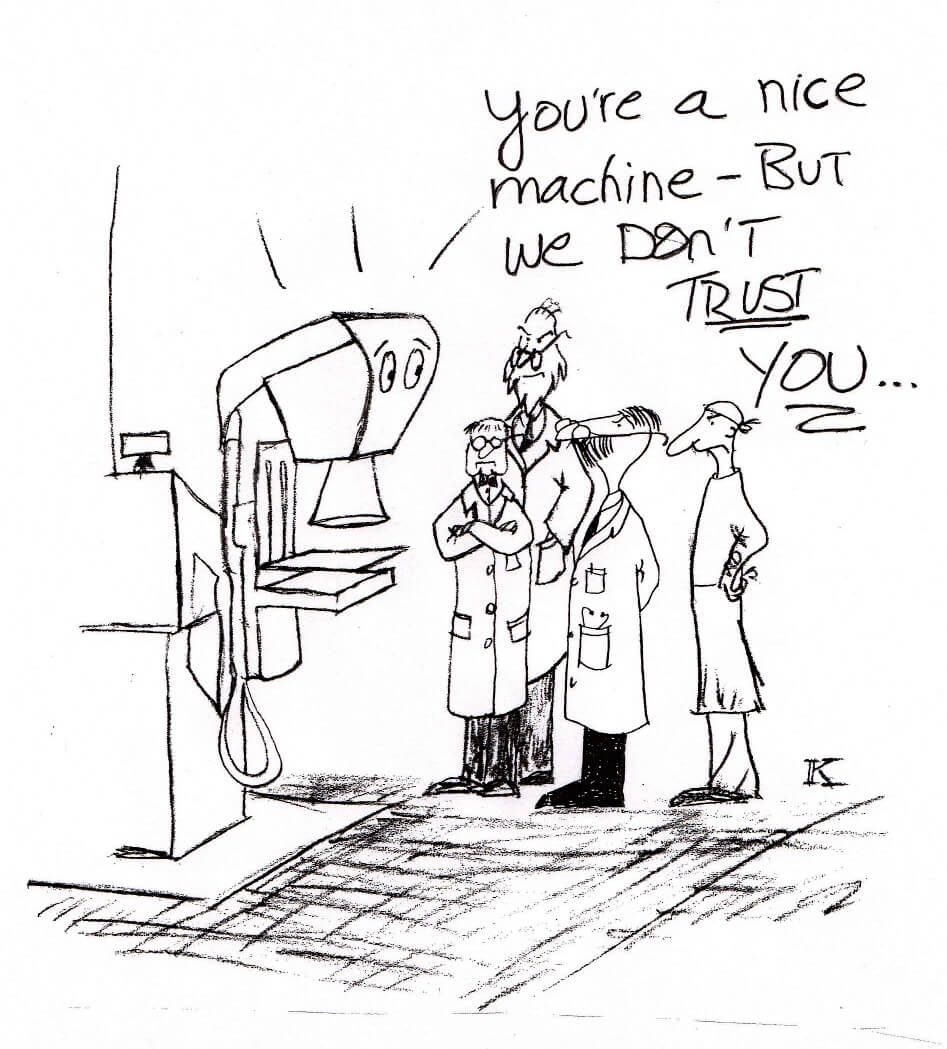
Dedicated to the initiative to reduce medical errors, we analyze classic mistakes in an engaging format we believe will maximize our reader’s likelihood of learning from those mistakes. Please go to the “About” link for our inspiration, our vision and our purpose.
We are posting two articles on the first of each month. Current articles are in the column to the right. Please check out our Article Archive Section for previous postings.
Announcement
The Witherspoon Institute will begin regular postings of articles, planning two a month, to be posted the 1st of the month.
We look forward to your comments and whatever feedback about our series you may wish to share.
Take care and be safe,
J.M. MacDavid, M.D.